Predictive Value of Serum Calprotectin Level in Nasal Polyposis

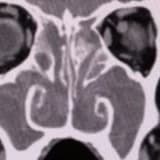
Predictive Value of Serum Calprotectin Level in Nasal Polyposis Asiye Merve Erdoğan1 , Talih Özdaş1 , Aykut Çakır1 , Sedat Alagöz1 , Kemal Koray Bal2 , Orhan Görgülü1 , Gökhan Kuran1 , Selçuk Matyar3 , Feride Fatma Görgülü4 1 Department of Otorhinolaryngology, Head and Neck Surgery, University of Health Sciences, Adana City Training and Research Hospital, Adana, Turkey 2Department of Otorhinolaryngology, Head and Neck Surgery, Mersin University Faculty of Medicine Hospital, Mersin, Turkey 3Department of Biochemistry, University of Health Sciences, Adana City Training and Research Hospital, Adana, Turkey 4Department of Radiology, University of Health Sciences, Adana City Training and Research Hospital, Adana, Turkey Cite this article as: Erdoğan AM, Özdaş T, Çakır A, et al. Predictive value of serum calprotectin level in nasal polyposis. B-ENT. 2023;19(3): 151-156. ABSTRACT Objective: Nasal polyps are benign intranasal masses that are usually bilateral, smooth-surfaced, gelatinous, originating from the epithelium in the middle meatus and ethmoid region, and can block the nasal passage. It is a chronic inflammatory disease of the nasal cavity and paranasal sinus mucosa with multifactorial etiology. Calprotectin (aka S100A8/A9, calgranulin A and B, alarmins, CLP) is a 36.5 small calcium- and zincbinding heterodimer released from macrophages and neutrophils. As an acute phase reactant, its release increases after inflammatory and infectious diseases and trauma. This study aimed to investigate the predictive value of serum calprotectin levels in nasal polyps. Methods: This prospective controlled study constitutes 40 nasal polyp patients, aged between 18 and 65 years, without any chronic systemic and inflammatory disease, and 40 healthy volunteers. Patients’ demographic data such as age and gender and the percentage of serum eosinophils in addition to calprotectin, mean platelet volume, leukocyte (white blood cell), hematocrit, total immunoglobulin E values, and neutrophil/ lymphocyte ratios in their venous blood samples were recorded for statistical comparison. Results: The calprotectin variable showed a statistically significant difference between the groups. Calprotectin values were higher in group I than in group II (P=.003). However, no significant correlation was found between endoscopic examination grade and calprotectin levels within group I (P=.827). Conclusions: High calprotectin level alone is a strong indicator of nasal inflammation, independent of the patient’s nasal polyp physical examination and paranasal sinus computed tomography (PNS CT) scores. It may be predicted that patients with high calprotectin levels will need more nasal and systemic steroid treatment. Keywords: Calprotectin, chronic rhinosinusitis, nasal polyps Introduction Nasal polyps (NPs) are benign intranasal masses that are usually bilateral, smooth-surfaced, gelatinous, originating from the epithelium in the middle meatus and ethmoid region, characterized by sinus or nasal mucosal chronic inflammation, and can block the nasal passage. It is also one of the most important causes of nasal congestion. Besides being the most common cause of nasal mass, it has been known for over 3000 years. Its prevalence in the population is approximately 0.2%- 4.3%.1 The NP is one of the most common problems in the otolaryngology (ear, nose, and throat [ENT]) clinic. Despite the abundance of studies on this disease, its etiology has not been fully determined, preventing an optimal level of treatment. Current treatments provide symptomatic treatment by eliminating the existing pathology rather than focusing on the etiology, and therefore often result in disease recurrence. Despite the many theories proposed for the development of NP, there is no definitive theory yet. Factors thought to play a role in the etiology are mucosal contact, Bernoulli phenomenon, chronic local infections, allergy, aspirin intolerance, asthma, genetic factors, and nasal mastocytosis.2 Nasal polyposis is a clinical manifestation of many immunological pathways and a local consequence of systemic diseases.3 Although its etiopathogenesis has not been fully elucidated, CC BY 4.0: Copyright@Author(s), “Content of this journal is licensed under a Creative Commons Attribution 4.0 International License.” Available online at www.b-ent.be Kuran et al. Predictive Value of Serum Calprotectin Level in Nasal Polyposis B-ENT 2023; 19(3): 151-156 152 its pathogenesis is related to the change in the balance between pro-inflammatory and anti-inflammatory cytokines.4 The respiratory epithelium provides a barrier to entry of pathogens through mucociliary function and tight junctions, and epithelial cells lining the airway respond to the presence of microorganisms by producing natural antimicrobial factors and mounting an inflammatory response. The epithelium is an essential part of the immune defense. Defects in a broad set of epithelial-related genes, in theory, could contribute to a dysfunctional innate immune response to environmental agents in the upper airways as they appear to do in the skin and lungs.5 Chronic rhinosinusitis (CRS) is commonly divided into 2 subtypes: CRS without nasal polyps (CRSsNP) and CRS with nasal polyps (CRSwNP). Sinonasal tissue from patients with CRSwNP displays a predominant infiltration of eosinophils (Eo) and T-helper type 2 (Th2) cytokines whereas CRSsNP tissue is characterized by more intense neutrophilic infiltration and a T-helper type 1-biased cytokine profile.5 Treatment of nasal polyposis usually requires multiple surgeries, and although various drugs are tried to control the disease, it is not always possible to provide a cure. Treatment of CRS is mostly glucocorticoid-based, but the response in the patients with NP is highly variable and oral corticosteroids have a limited place in the treatment due to their side effects in long-term use. Some patients with NPs show high resistance to corticosteroid therapy, highlighting the need for therapeutics to address corticosteroid-refractory pathophysiological mechanisms involved in NP.6 With the discovery of non-invasive biomarkers in NP, it will be possible to obtain prognostic information and provide targeted medical therapy. Immunoglobulin E (IgE), an inducer of eosinophilia, has been investigated as a biomarker for CRS phenotyping and treatment. However, the anti-IgE therapeutic omalizumab improved sinus computed tomography (CT) scores and reduced NP size in patients with CRSwNP, but a reduction in nasal mucosal inflammation was not conclusively seen.7 While the benefit of interleukin-5 antagonists in asthmatic patients with eosinophilia and the Th2 phenotype has been well demonstrated,8 they have also shown a reduction in NP size and a reduced need for revision surgeries. However, they did not conclusively show improvement in nasal symptom scores.9 Two myeloid-related proteins, MRP-8 (S100A8) and MRP14 (S100A9), belong to the S100 family of calcium-binding proteins.10 The S100A8 and A9 and their complex form, calprotectin,11 are often used interchangeably. Calprotectin (aka S100A8/A9, calgranulin A and B, alarmins, CLP) is a 36.5 small calcium- and zinc-binding heterodimer released from macrophages and neutrophils. It usually binds to its main receptor TLR4. The S100A8/A9 is expressed and secreted primarily by neutrophils and macrophages, accounting for 45% of all cytosolic proteins in neutrophils. As an acute phase reactant, its release increases after inflammatory and infectious diseases and trauma. Meanwhile, neutrophils and other cells are induced to express reactive oxygen species, cytokines, and nitric oxide. Calprotectin is a potential biomarker in inflammatory diseases due to its stability at room temperature. Its concentration in various body fluids (feces, serum, saliva, etc.) has been reported, showing that serum levels in healthy individuals are usually below 1 μg/mL and increase 100-fold after inflammation. Calprotectin has a documented half-life of 5 hours, and unlike other acute phase reactants produced in the liver, calprotectin is locally synthesized and secreted at the inflammation site. Calprotectin is hypothesized to activate both anti-inflammatory and pro-inflammatory signals, thereby modulating the immune system.12 Elevated expression of S100A9, MMP3, MMP7, MMP11, MMP25, MMP28, and CTSK was observed in tissue from CRSwNP compared to control tissue. The S100A9 stimuli induce nasal epithelial cell proliferation in an MMP3-dependent manner.5 Although it has been reported that some MMP types and CTSK are affected by external factors such as smoke inhalation,6 there is no similar data for calprotectin. Our study aimed to investigate the predictive value of serum calprotectin levels in NP and to give an idea for noninvasive methods in diagnosis and treatment. Methods This prospective controlled study constitutes 40 NP patients, aged between 18 and 65 years, without any chronic systemic and inflammatory disease, who applied to Adana City Training and Research Hospital ENT outpatient clinic as group I and 40 healthy volunteers as group II. Clinical Research Ethics Committee approval was obtained from Ethics Committee of Health Sciences University, Adana City Training and Research Hospital (Date: 17.06.2020 No:946). Attention was paid to ensure that the patients did not receive systemic steroid treatment in the last month and did not have an acute infectious disease. Patients were evaluated for the Samter triad, and patients with known aspirin sensitivity and a diagnosis of asthma were excluded. It was ensured that the control group did not have any acute or chronic infectious inflammatory disease and did not use drugs. Those with abnormal infection or biochemical parameters in their blood samples were excluded from the study. In addition, individuals under the age of 18 or over the age of 65, those with inverted papilloma, cystic fibrosis, sinonasal granulomatosis, any autoimmune disease, history of acute or chronic infection or infection symptoms, obesity, hypertension, angina pectoris, myocardial Main Points • High serum calprotectin level alone is a strong indicator of nasal inflammation. • High serum calprotectin levels are independent of the patient’s nasal polyp physical examination and paranasal sinus computed tomography (PNS CT) scores. • It may be predicted that patients with high calprotectin levels will need more nasal and systemic steroid treatment. B-ENT 2023; 19(3): 151-156 Kuran et al. Predictive Value of Serum Calprotectin Level in Nasal Polyposis 153 infarction, diabetes mellitus, metabolic syndrome, obstructive sleep apnea syndrome, chronic obstructive pulmonary disease, amyloidosis, chronic kidney failure, or cancer history, those who used oral corticosteroids in the last month, and pregnant women were also excluded from the study. Endoscopy stages of NP patients evaluated with 0° and 30° 4-mm or 2.7-mm rigid endoscopes in our outpatient clinic were evaluated. Physical examination findings were scored with a scale of 0-3 (endoscopic view of polyps) for both nasal cavities (right/left) as defined by Lildholdt et al13 (Table 1). The Lund–Mackay CT staging used in NP patients in the study includes scoring the bilateral sinus opacification area from 0 to 2 for a possible score range of 0 to 24 (Table 2).14 Patients’ demographic data such as age and gender and the percentage of serum Eo in addition to calprotectin, mean platelet volume (MPV), leukocyte (white blood cell [WBC]), hematocrit, total IgE values, and neutrophil/lymphocyte ratios in their venous blood samples were recorded for statistical comparison. Extra venous blood samples were collected from patients during routine laboratory tests and transferred into anticoagulant-free 5.0 mL vacuum collection tubes (Becton Dickinson Vacutainer® ref. 367955) for serum separation under standard conditions to minimize sources of preanalytical variation. All blood samples with visible hemolysis were discarded. Anticoagulant-free tubes were allowed to clot for 15-20 minutes at room temperature and were separated by centrifugation at 3000 rpm for 15 minutes. Samples were frozen (−80°C). Once all samples were ready, they were thawed, mixed, centrifuged again (15 minutes at 3000 rpm), and analyzed at room temperature. Serum samples were thawed once. The collected serum samples were analyzed using a Human Calprotectin Enzyme-Linked Immunosorbent Assay kit (Catalog Number: SEK504Hu). After terminating the assay with an enzyme substrate following the manufacturer’s instructions (CLOUD-CLONE CORP, Wuhan, PR China), the reaction in samples was measured spectrophotometrically with Awareness Technology (Palm City, Fla, USA) at a wavelength of 450 nm. The detection ranges of these kits were 31.20-2000 pg/mL for calprotectin. The minimum detectable calprotectin dose is less than 13.6 pg/mL. Patients’ calprotectin levels, measured as picograms/milliliter, were converted to nanograms/milliliter. Statistical Analysis After creating a database using the Statistical Package for Social Sciences (SPSS) for Windows 11.5 software package (SPSS Inc.; Chicago, IL, USA), the data collected through the patient follow-up forms were transferred to the electronic environment and evaluated. Descriptive statistics were presented as number (n) and percentage (%) for categorical variables, as mean ± standard deviation for numerical parameters meeting parametric test assumptions, and median and minimum–maximum values for those that do not. The conformity of the data to the normal distribution was evaluated with the Shapiro–Wilk normality test. Numerical variables were compared between groups using the “Student”s t-test” if parametric test assumptions were met, and the “Mann–Whitney U-test” if not. The relationship between the ordinal variable and calprotectin levels was evaluated using the Spearman correlation test. The SPSS 16.0 software for Windows (SPSS, Inc., Chicago, IL, USA) was used for all statistical analyses, and P < .05 was considered statistically significant. Results Approval for our study was obtained from the Clinical Research Ethics Committee of Adana City Training and Research Hospital with the decision dated 17.06.2020 and numbered 946. Volunteers were informed about our study and their consent was obtained. A total of 76 people, including 37 patients with NP (group I) and 39 healthy volunteers without any disease (group II), were included in our study. Of 37 patients in group I, 16 (43.2%) were female and 21 (56.8%) were male. The age of the patients ranged from 18 to 65, with a mean age of 37.05+13.023 (Tables 3 and 4). According to the 0-3 scale (endoscopic view of polyps) defined by Lildholdt et al13 the physical examination scores in the right/left nasal cavity were recorded as a minimum of 1/1 and a maximum of 3/3. Lund–Mackay scores on paranasal sinus computed tomography (PNS CT) imaging ranged from 4 to 24, with a mean of 15.70 ± 5.995. The serum calprotectin levels of group I ranged from 0 to 67, with a mean of 15.86 ± 17.769. A statistically significant relationship was found between leukocyte and calprotectin levels (r=0.330, P < .00). Patients with high calprotectin levels had higher blood leukocyte levels. There was a statistically significant relationship between the grade of endoscopic examination and the percentage of Eo (r=0.357, P < .00). The percentage of blood Eo was higher in patients with a high NP physical examination grade. Table 1. The Scale of 0-3 (Endoscopic View of Polyps) for Both Nasal Cavities (Right/Left) as Defined by Lildholdt et al13 Endoscopic View of Polyps Scale No polyps 0 Limited polyp in middle meatus 1 Polyp below the middle turbinate 2 Diffuse nasal polyposis 3 Table 2. The Lund–Mackay CT Staging14 Localization Right Nasal Cavity Left Nasal Cavity Maxillary sinus (0, 1, 2) Anterior ethmoid cells (0, 1, 2) Posterior ethmoid cells (0, 1, 2) Sphenoid sinus (0, 1, 2) Frontal sinus (0, 1, 2) Osteomeatal complex (0, 2)* 0*, normal; 0, normal; 1, partial opacification; 2*, total opacification; 2, total opacification. Kuran et al. Predictive Value of Serum Calprotectin Level in Nasal Polyposis B-ENT 2023; 19(3): 151-156 154 There was a statistically significant relationship between Lund– Mackay score and neutrophil/lymphocyte ratio (r=−0.375, P < .00). Patients with a high PNS CT score also had a high neutrophil/lymphocyte ratio. There was a statistically significant relationship between the Lund–Mackay score and the endoscopic examination grade (r=0.738, P < .00). Physical examination NP grade and Lund– Mackay scores were correlated with each other. However, there was no significant correlation between the patients’ endoscopic examination grade and serum calprotectin levels (P=.827) and between Lund–Mackay score and serum calprotectin levels (P=.327). Group II consisted of 39 healthy volunteers, 21 (53.8%) female and 18 (46.2%) male. The age of the patients in group II ranged from 18 to 53, with a mean of 30.56 ± 8.488. Serum calprotectin levels of group II ranged from 0 to 18, with a mean of 4.72 ± 3.692. Two groups were compared for the laboratory parameters: serum calprotectin level, Eo percentage, MPV, leukocyte value (WBC), hematocrit, and neutrophil/lymphocyte ratio. The calprotectin variable showed a statistically significant difference between the groups. Calprotectin values were higher in group I than in group II (P=.003). But, there was no significant relationship between endoscopic examination grade and calprotectin levels within group I (P=.827). The Eo percentage variable showed a statistically significant difference between the groups. Group I had a higher percentage of Eo than group II (P=.001). The MPV variable showed a statistically significant difference between the groups. The MPV value of group I was higher than group II (P=.002). The neutrophil/lymphocyte ratio variable showed no statistically significant difference between the groups (P=.620). There was no statistically significant difference between the serum calprotectin levels and neutrophil/ lymphocyte ratio variable. Discussion While the prevalence of nasal polyposis was reported to be 1%-1.3% on average in European populations,15 Erbek et al16 determined the prevalence of NP in the Turkish population as 2.7%. Although the onset age of NP is 2 years, it is very rare (0.1%) before the age of 10. It is most common between the ages of 30 and 40 and is seen twice as often in men than as in women.17 Although the incidence of NP increases every 10 years between the ages of 20 and 60, it decreases again Table 3. Group I Descriptive Statistics Group I n Minimum Maximum Mean Standard Deviation Statistic Statistic Statistic Statistic Standard Error Statistic Age 37 18 65 37.05 2.141 13.023 Calprotectin 37 0 67 15.86 2.921 17.769 Eo % (0.8-8) 37 0 14 5.22 0.495 3.010 MPV (7.5-11.5) 37 7 11 8.41 0.147 0.896 Leukocyte 37 3800 10,000 7267.57 220.770 1342.894 Hematocrit 37 28 48 41.03 0.755 4.592 NEU/LYMP 37 1 4 2.16 0.153 0.928 Nasal polyp grade 0-3 37 11 33 20.89 0.919 5.592 Lund–Mackay score 37 4 24 15.70 0.986 5.995 Valid N (listwise) 37 Eo, the percentage of serum eosinophils; MPV, mean platelet volume; NEU/LYMP, neutrophil/lymphocyte ratios. Table 4. Group II Descriptive Statistics Group II n Minimum Maximum Mean Standard Deviation Statistic Statistic Statistic Statistic Standard Error Statistic Age 39 18 53 30.56 1.359 8.488 Calprotectin 39 0 18 4.72 0.591 3.692 Eo % (0.8-8) 39 1 10 3.13 0.355 2.215 MPV (7.5-11.5) 38 8 10 9.03 0.133 0.822 Leukocyte 39 3700 11,000 6664.10 270.888 1691.696 Hematocrit 39 30 55 40.21 0.747 4.663 NEU/LYMP 39 0 6 2.10 0.175 1.095 Valid N (listwise) 38 Eo, the percentage of serum eosinophils; MPV, mean platelet volume; NEU/LYMP, neutrophil/lymphocyte ratio. B-ENT 2023; 19(3): 151-156 Kuran et al. Predictive Value of Serum Calprotectin Level in Nasal Polyposis 155 after the age of 60.18 Of 37 patients in group I, 16 (43.2%) were female and 21 (56.8%) were male. Although the gender distribution of our sample was similar to the literature, our patient group was younger than in other similar studies. In the study of Yenigün19 in 2015, in which 80 patients with recurrent NP and 78 patients with non-recurrent NP of allergic origin were included, preoperative neutrophil, Eo, neutrophil/lymphocyte, and Eo/lymphocyte values were significantly higher in patients with recurrent NP, and it was suggested that neutrophil/lymphocyte and Eo/lymphocyte values could be used as an auxiliary method in deciding the necessity of relapse follow-up in the patients with nasal polyposis. Also in our study, the percentage of Eo in the patient group was higher compared to the control group (P=.001). But no correlation was found between the percentage of Eo and PNS CT scores (P=.327). In the study of Kara et al20 in which they compared nasal polyposis patient and control groups in 2018, statistically significant correlation was found between nasal polyposis severity and Eo/lymphocyte ratio, while neutrophil/lymphocyte, throm bocyte/lymphocyte, Eo/lymphocyte ratios, and erythrocyte distribution width values were not statistically significant in terms of recurrence. Also in our study, the neutrophil/lymphocyte ratio variable showed no statistically significant difference between the groups. There was no statistically significant difference between the neutrophil/lymphocyte ratio and calprotectin levels (P=.620). The neutrophil/lymphocyte ratio does not seem to be a marker of inflammation unlike calprotectin. There are many studies in the literature investigating the relationship between calprotectin levels and ENT diseases. In their 2020 study with 44 participants, Kuzucu et al21 found that the serum calprotectin levels of patients with idiopathic sudden sensorineural hearing loss were higher than the controls and serum calprotectin value of patients who did not recover from the idiopathic sudden sensorineural hearing loss was found to be significantly higher than those with partial or complete recovery. In a study conducted by Spiekermann et al22 in 2017 with 25 acute tonsillitis patients, 36 peritonsillar abscess patients, 16 peritonsillar cellulitis patients, and 15 healthy volunteers, the serum calprotectin levels of peritonsillar abscess patients were statistically significantly higher than in peritonsillar cellulitis patients and healthy controls. Similarly, serum calprotectin levels of acute tonsillitis patients were statistically significantly higher than controls. In the analysis of salivary calprotectin levels, no significant difference was observed between acute tonsillitis and peritonsillar cellulitis patients. Also, C-reactive protein (CRP) and white blood cell levels did not differ between the diagnostic groups. Although increased CRP levels (>15.5 mg/dL) and age>35 years were defined as predictors of retropharyngeal abscesses and necrotizing fasciitis, they concluded that neither CRP nor leukocytes in the serum were appropriate distinguishing markers. In conclusion, it is claimed that high calprotectin (S100A8/ A9) levels in the serum and saliva of peritonsillar abscess patients represent a new application of the well-known biomarker calprotectin.22 In their 2016 study, Van Crombruggen et al23 examined serum calprotectin levels in NP patients. They found that cellular calprotectin was transferred to the extracellular matrix due to inflammation and therefore was elevated in serum. In their 2020 study with 26 CRSs with NP and 24 without NP and 27 control groups, Candar et al24 found that serum calprotectin levels were statistically significantly higher in CRSwNP patients than in nonpolyposis and healthy individuals, and serum calprotectin levels were higher in patients with Samter’s triad. They attributed this to the more severe complaints of asthma-triggering inflammation and NP in Samter’s triad patients.24 They also found a relationship between the Nose Obstruction Symptom Evaluation (NOSE) scale scores and serum calprotectin values and showed that nasal obstruction complaints increased in patients with CRS, especially those presenting with NPs, consequently leading to an increase in serum calprotectin levels.24 Also in our study, serum calprotectin levels, a marker of inflammation, were found to be significantly higher in the CRS patients with NP compared to healthy controls. The phenotypic differentiation of CRS based on the presence or absence of inflammatory polyps continues to be discriminators of response to medical and/or surgical treatment to date. The emergence of biologics in the treatment of atopic disease and asthma, and perhaps a new look at topical treatments for CRS, has placed a new emphasis on understanding the pathophysiology of inflammatory sinus polyp pathogenesis.6 Considering that high calprotectin levels alone are a strong indicator of nasal inflammation, independent of the patients’ NP physical examination and PNS CT scores, it may be predicted that the patients with high calprotectin levels will need more nasal and systemic steroid treatment. In order to obtain more detailed prognostic information, studies with larger series in which patients are evaluated preoperatively and postoperatively are needed. Ethics Committee Approval: Clinical Research Ethics Committee approval was obtained from Ethics Committee of Health Sciences University, Adana City Training and Research Hospital (Date: 17.06.2020 No:946). Informed Consent: The clinical, radiological and laboratory details of the patients were reviewed after obtaining informed consent. Peer-review: Externally peer-reviewed. Author Contributions: Concept – A.M.E.; Design – A.M.E., T.Ö.; Supervision – T.Ö., S.A., K.K.B., O.G.; Funding – A.M.E., O.G.; Materials – A.M.E., A.Ç., O.G., G.K., S.M., F.F.G.; Data Collection and/or Processing – A.M.E., A.Ç., O.G., G.K., S.M., F.F.G.; Analysis and/or Interpretation – T.Ö., K.K.B., G.K., S.M., F.F.G.; Literature Review – A.M.E., A.Ç., S.A.; Writing – A.M.E., T.Ö., K.K.B.; Critical Review – A.M.E., S.A., K.K.B. Declaration of Interests: The authors have no conflict of interest to declare. Funding: This study received no funding. Kuran et al. Predictive Value of Serum Calprotectin Level in Nasal Polyposis B-ENT 2023; 19(3): 151-156 156 References 1. Brain TJ. Historical background of nasal polyps. In: Settipane G, Lund V, Berstein J, Tos M, eds. Nasal Polyps, Epidemiology, Pathology, Treatment. RI: Oceanside Publications; 1997:7-15. 2. Önerci M. Burun poliplerinin patogenezi. In: Önerci M., Polipozis N., eds. Hacettepe Üniversitesi Hastaneleri Basımevi. Ankara; 2006:7-14. 3. Van Zele T, Gevaert P, Watelet J, et al. Staphylococcus aureus colonization and IgE antibody formation to enterotoxins is increased in nasal polyposis. J Allergy Clin Immunol. 2004;114(4):981-983. [CrossRef] 4. Choi MS, Ray R, Zhang Z, Mukherjee AB. INF-gamma stimulates the expression of a novel secretoglobin that regulates chemotactic cell migration and invasion. J Immunol. 2004;172(7):4245-4252. [CrossRef] 5. Tieu DD, Peters AT, Carter RG, et al. Evidence for diminished levels of epithelial psoriasin and calprotectin in chronic rhinosinusitis. J Allergy Clin Immunol. 2010;125(3):667-675. [CrossRef] 6. Workman AD, Kohanski MA, Cohen NA. Biomarkers in chronic rhinosinusitis with nasal polyps. Immunol Allergy Clin North Am. 2018;38(4):679-692. [CrossRef]. Epub 2018 Sep 21. 7. Gevaert P, Calus L, Van Zele T, et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J Allergy Clin Immunol. 2013;131(1):110-6.e1. [CrossRef] 8. FitzGerald JM, Bleecker ER, Nair P, et al. Benralizumab, an antiinterleukin-5 receptor alpha monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128-2141. [CrossRef] 9. Gevaert P, Van Bruaene N, Cattaert T, et al. Mepolizumab, a humanized anti-IL-5 mAb, as a treatment option for severe nasal polyposis. J Allergy Clin Immunol. 2011;128(5):989-95.e1 e1–8. [CrossRef] 10. Kerkhoff C, Vogl T, Nacken W, Sopalla C, Sorg C. Zinc binding reverses the calcium-induced arachidonic acid-binding capacity of the S100A8/A9 protein complex. FEBS Lett. 1999 October 22;460(1):134-138. [CrossRef] 11. SHIBATA F, Ito A, OHKUMA Y, MITSUI K-i. Mitogenic activity of S100A9 (MRP-14). Biol Pharm Bull. 2005;28(12):2312-2314. [CrossRef] 12. Udeh R, Advani S, de Guadiana Romualdo LG, Dolja-Gore X. Calprotectin, an emerging biomarker of interest in COVID-19: a systematic review and meta-analysis. J Clin Med. 2021;10(4):775. [CrossRef] 13. Lildholdt T, Rundcrantz H, Bende M, Larsen K. Glucocorticoid treatment for nasal polyps. The use of topical budesonide powder, intramuscular betamethasone, and surgical treatment. Arch Otolaryngol Head Neck Surg. 1997;123(6):595-600. [CrossRef] 14. Brooks SG, Trope M, Blasetti M, et al. Preoperative Lund-Mackay computed tomography score is associated with preoperative symptom severity and predicts quality-of-life outcome trajectories after sinus surgery. Int Forum Allergy Rhinol. 2018;8(6):668-675. [CrossRef] 15. Hosemann W, Göde U, Wagner W. Epidemiology, pathophysiology of nasal polyposis, and spectrum of endonasal sinus surgery. Am J Otolaryngol. 1994;15(2):85-98. [CrossRef] 16. Erbek SS, Yurtcu E, Erbek S, Atac FB, Sahin FI, Cakmak O. Proinflammatory cytokine single nucleotide polymorphisms in nasal polyposis. Arch Otolaryngol Head Neck Surg. 2007;133(7):705-709. [CrossRef] 17. Drake-Lee AB. Medical treatment of nasal polyps, rhinology. Internation J. 1994;32:1-4. 18. Boruk M, Railwah C, Lora A, et al. Elevated S100A9 expression in chronic rhinosinusitis coincides with elevated MMP production and proliferation in vitro. Sci Rep. 2020;10(1):16350. [CrossRef] 19. Yenigün A. Assessment of patients with nasal polyposis by the neutrophil-to-lymphocyte ratio and eosinophil-to-lymphocyte ratio. Kulak Burun Bogaz Ihtis Derg. 2015;25(4):193-199. [CrossRef] 20. Kara A, Guven M, Yilmaz MS, Demir D, Elden H. Are neutrophil, platelet and eosinophil-to-lymphocyte ratio and red blood cell distribution width can be used for nasal polyposis? Eur Arch Otorhinolaryngol. 2018;275(2):409-413. [CrossRef]. Epub 2017 Nov 30. 21. Kuzucu İ, Çandar T, Baklacı D, et al. A prognostic marker in idiopathic sudden sensorineural hearing loss: serum calprotectin. Clin Exp Otorhinolaryngol. 2020;13(1):36-40. [CrossRef] 22. Spiekermann C, Russo A, Stenner M, Rudack C, Roth J, Vogl T. Increased levels of S100A8/A9 in patients with peritonsillar abscess: a new promising diagnostic marker to differentiate between peritonsillar abscess and peritonsillitis. Dis Markers. 2017;2017:9126560. [CrossRef] 23. Van Crombruggen K, Vogl T, Pérez-Novo C, Holtappels G, Bachert C. Differential release and deposition of S100A8/A9 proteins in inflamed upper airway tissue. Eur Respir J. 2016;47(1):264-274. [CrossRef] 24. Candar T, Baklaci D, Kuzucu I, Kayabasi S. A proinflammatory marker in chronic rhinosinusitis: serum calprotectin. Acta Biochim Pol. 2020;67(3):367-371. [CrossRef]